Laser Haemorrhoid Treatment (LHP)
Can haemorrhoids be lasered?
Haemorrhoidoplasty: Treat haemorrhoids with laser
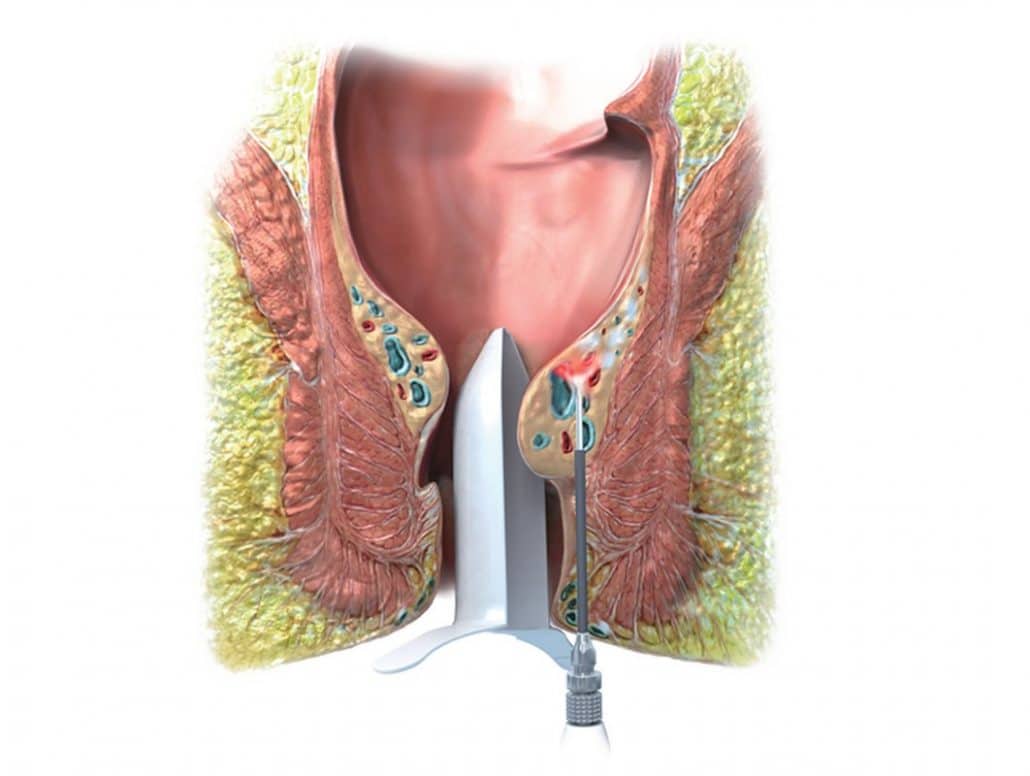
Laser treatment of dilated vascular structures has long been proven in the treatment of varicose veins (varices). In proctology, haemorrhoid treatment with an 810 nm laser was first reported in 2009 by Hèlio Plapler at the University Hospital of Sao Paulo. The development of a fine, cone-shaped radiating glass fibre probe and the use of a waveform-optimised 1470 nm laser improved the effectiveness of the laser application.
Haemorrhoidoplasty (LHP) can be considered a mature therapy procedure today. In this procedure, the haemorrhoidal nodes are reduced in size and fixed from the inside with dosed laser energy. The Hemorrhoid Laser Procedure (HeLP), which only scleroses the afferent vessels at the base of the haemorrhoid, is even more restrained.
When the treatment-related swelling has subsided after one to two weeks, the haemorrhoidal nodes shrink and no longer tend to prolapse. This method can additionally be combined with gathering fixation sutures(HAL-RAR) if a pronounced prolapse is to be treated.
In other words, the dilation of the haemorrhoidal vessel (vascular component of haemorrhoidal disease) is treated with laser and the mechanical instability (prolapse component) is treated with suturing. These two therapeutic principles interact synergistically ("belt and braces principle").
What do I get out of it as a patient?
Laser treatment of haemorrhoids: Major advantages
- The procedure is performed on an outpatient basis, after 2 hours of monitoring in the recovery room you can be picked up again
- LHP can also be used in stage 3 and - with restrictions - stage 4 haemorrhoidal disease.
- Larger wounds as with conventional haemorrhoid removal are avoided
- The downtime in work and sports is minimal compared to conventional surgery, most patients are fit for work again after 5 - 7 days.
- Studies showed better efficacy and quality of life after laser haemorrhoidoplasty compared to the commonly used rubber band ligation
- The haemorrhoidal cushion, which is important for elasticity, sensitivity and sealing against gas and fluid of the anus, is preserved and reduced to the normal level.
- The sphincter muscle is optimally protected
Statutory health insurance
Laser treatment: Does the health insurance cover the costs?
Before you read on, you probably want to know whether the treatment costs are covered by health insurance. To date, the innovative treatment procedures with lasers are not included in the standard care.
The good news is that a whole series of statutory health insurers, predominantly from the group of company health insurance funds (BKKs), have now concluded contracts with us within the framework of integrated care (IGV). For the insured of these health insurance companies we can therefore offer a modern laser operation without additional costs for the patient. Information on the various modalities of reimbursement and assumption of treatment costs by health insurance can be found here.
A safe procedure with few complications
Laser haemorrhoidoplasty (LHP): Are there risks?
Our experience shows that laser haemorrhoidoplasty is a very safe and effective procedure, especially when compared to other haemorrhoid surgery techniques.
- Postoperative bleeding from the laser channels can occur, but is never dangerous and can usually be stopped by applying gentle pressure.
- Local swelling and anal thrombosis are not uncommon in the first 1 to 2 weeks, but will go away on their own.
- Bacterial inflammations up to fistula formation could be imagined, but have not been observed so far.
- Especially in our preferred combination with HAL-RAR, very good long-term results can be expected. 90 % of the treated patients are symptom-free after 3 years.
The individual steps of the treatment
Laser haemorrhoidoplasty (LHP): Treatment procedure
Find out here what is important for the smooth course of treatment during laser haemorrhoid surgery. General information on outpatient rectal surgery can also be found on our page "Outpatient haemorrhoid surgery".
Anamnesis (previous history) - and assessment of findings
At your first appointment in our practice, you will tell us about the duration, type and intensity of your symptoms. The examination clarifies whether enlarged haemorrhoids are actually responsible for these symptoms. At least half of all patients who present with "haemorrhoids" are actually suffering from anal fissure or anal eczema independent of the rectum.
Discussion of the alternatives
Is laser haemorrhoidoplasty the optimal procedure for you and your condition? In principle, haemorrhoids from I° - III° can be treated with it. In the case of individual, very large lumps, conventional haemorrhoid removal may be the method of choice.
If a patient has only few symptoms, it is sometimes possible to avoid surgery altogether and only treat symptomatically with stool regulation and ointment. In the case of very pronounced, circulating findings, a stapler haemorrhoidopexy (Longo operation) may be useful in individual cases.
Once these questions have been clarified, we will inform you about the expected impairments and possible, albeit rare, complications. The consultation ends with the signing of the written consent form for the operation.
Anaesthesia talk ("premedication")
For this purpose, you should visit the IATROS clinic a few days before the planned procedure or contact us by telephone, but at the latest one day before. Please bring the completed information/questionnaire with you. If possible, bring an interpreter with you if you do not feel confident in the German or English language.
When: Monday to Thursday from 9:00 to 17:00 and Friday from 9:00 to 13:00 without appointment. The IATROS clinic is closed on bridge days and public holidays.
Where? Joint practice for anaesthesia IATROS-KLINIK GmbH, Dr. med. Javier del Valle, Dr. med. Michael Kaspar, Dr. med. Christoph Schmitt-Hausser
Nymphenburger Straße 1, 80335 Munich, (high-rise building opposite Löwenbräu-Keller, U1/U7 Stiglmairplatz, tram line 22), Tel.: 089 - 461356-0
For further information, please visit the clinic's website at https://www.iatros-klinik.de/information/.
Preparation for surgery
- Examinations by the general practitioner: Healthy patients up to 60 years of age do not need any special preliminary examinations. In individual cases, the anaesthetist may order necessary examinations. Healthy patients over 60 years of age should bring their existing examination results, ECG and laboratory with them. In the case of chronic illnesses with performance limitations as well as cardiovascular events in the last 12 months (heart attack, stroke), we advise against outpatient surgery and would recommend surgery in an appropriately equipped acute hospital.
- If you have to take "blood thinning" medication: With any permanent medication, please talk to your family doctor and the anaesthetist about the use before and after the operation! Operations with a slightly increased risk of bleeding can be performed with ASA (Aspirin®). If it is not necessary, ASA should be discontinued 5 days before the operation and only taken again after one week. We advise against outpatient surgery with clopidogrel (Plavix®), phenprocoumon (Marcumar®) and the new oral anticoagulants (NOAKs).
- Medication for diabetes: Please discuss with the anaesthetist whether metformin should be paused and whether and when insulin should be injected.
- Corona test: As of 14.09.21, the 3 G regulation applies until further notice, a PCR test is no longer mandatory. For convalescents whose infection occurred more than 6 months ago and unvaccinated persons, a PCR test no older than 72 hours with subsequent quarantine at home is still mandatory.
- Bowel preparation: Bowel irrigation as for colonoscopy is not necessary for proctological operations.
- Prescriptions for painkillers and other medicines required during follow-up treatment will be given to you when you make your appointment. Please inform us of any known incompatibilities. If you take medication regularly, we will need to check our prescription for interactions. Get these medicines so that you are already equipped on the evening of the operation.
- Certificate of incapacity for work (AU): If you are a professional or student and require a certificate of incapacity for work, please also inform us of this when making your appointment.
Important: Organise a pick-up!
Even if you feel fully recovered after the procedure and the anaesthetic has worn off - we must not let you go home alone. Circulatory reactions or anaesthetic after-effects ("rebound") could put you in danger. You are therefore not allowed to go home alone, not even on public transport.
It is mandatory that an adult person picks you up at the Iatros Clinic. Please organise the pick-up reliably for the planned discharge date.
On the day of the operation at the IATROS clinic (always Friday at our clinic)
Before the operation:
- 6 hours before the planned start of the operation you must remain sober, i.e. you must not eat, drink, smoke, suck or chew anything. The only exception is that you take your medication at the usual time with a sip of water. If in doubt, discuss the procedure with the anaesthetist. You may drink clear water by the sip up to 3 hours before the scheduled operation.
- In the excitement, do not forget to visit the toilet again. If you are prone to constipation and do not have regular bowel movements in the morning, we recommend using an enema on the morning of the day of the operation (Klysma saline, available over the counter at the pharmacy).
- In case of acute illnesses, e.g. cold, febrile infections or diarrhoea, the operation cannot be performed. Please inform us as soon as possible.
- Please refrain from wearing make-up, lipstick and nail varnish. Leave jewellery, large sums of money and valuables at home! The IATROS clinic accepts no liability for these items.
Be on time for the operation! As the duration of an operation can never be predicted with absolute certainty in advance, there may be delays in the start of the operation, we ask for your understanding.
After the operation:
- The anaesthetic is over. In the recovery room you will be monitored and cared for with regard to your circulatory function and breathing. As soon as you are fully awake again, you will be given a cup of tea and a biscuit as a little refreshment. Then you should also go to the toilet to urinate. The anaesthetist will then decide when the person who is to collect you can meet you. The person collecting you will be informed by telephone.
- Have yourself taken home by the direct route. Especially for male patients over the age of 50, we recommend going to the toilet again at the latest then, so that the bladder does not become overfull. If you have a general tendency to urinate frequently or have a weakened urine stream, we would prescribe a medication (Tamsulosin ®) as a preventive measure to facilitate urination.
- In case of problems: On the second page of our information sheet on the Iatros Clinic you will find my mobile phone number in red letters, which you can dial for all urgent matters. For simple queries without any particular urgency, I would ask you to choose the email route.
The first days after the operation
- ...to be continued
10 days after the operation
Hemorrhoids: Further treatment methods
In addition to haemorrhoidoplasty, haemorrhoid artery ligation with Recto-Analer Reconstruction (HAL-RAR) is also a promising therapy method that we use in our proctological center in Munich. The hemorrhoid nodes are not removed, but the arterial influx to them is prevented.
Hemorrhoidectomy is a conventional therapy method that is usually performed with an electric scalpel. In order to achieve even better results and accelerate wound healing, we recommend hemorrhoidectomy with laser instead of electrical scalpel.
Dr Hofer and Dr Bärtl are specialists in the treatment of haemorrhoids. Come to our proctology practice and let us advise you in detail. We are happy to be there for you.
Bibliography: Laser haemorrhoidoplasty
Bachtsetzis, .G., Bachtsetzis, .C., El Dakroury, .N., & Athanasiou, .G. (2019). ELITE: a diode laser minimally invasive technique for hemorrhoids during surgical treatment for anal fissure. Journal of Surgical Case Reports, 2019(1),
Herold, A. (2009). Comment by A. Herold on R. Salfi A New Technique for Ambulatory Hemorrhoidal Treatment. Doppler-Guided Laser Photocoagulation of Hemorrhoidal Arteries. coloproctology, 31(2), 104-104.
Kahlke, V. (2012). Randomized Trial of the Hemorrhoid Laser Procedure vs Rubber Band Ligation 6-Month Follow-Up. Diseases of the Colon & Rectum, 55(4), e45-e45.
Maloku, H., Gashi, Z., Lazovic, R., Islami, H., & Juniku-Shkololli, A. (2014). Laser Hemorrhoidoplasty Procedure vs Open Surgical Hemorrhoidectomy: a Trial Comparing 2 Treatments for Hemorrhoids of Third and Fourth Degree. Acta Informatica Medica, 22(6), 365-367.
Nardi, P., Tamburini, A., Gazzetta, P., Lemma, M., Pascariello, A., & Asteria, C. (2016). Hemorrhoid laser procedure for second- and third-degree hemorrhoids: results from a multicenter prospective study. Techniques in Coloproctology, 20(7), 455-459.
Plapler, H., Hage, R., Duarte, J., Lopes, N., Masson, I., Cazarini, C., & Fukuda, T. (2009). A New Method For Hemorrhoid Surgery: Intrahemorrhoidal Diode Laser, Does It Work?. Photomedicine and Laser Surgery, 27(5), 819-823.
Poskus, T., Danys, D., Makunaite, G., Mainelis, A., Mikalauskas, S., Poskus, E., Jotautas, V., Dulskas, A., Jasiunas, E., & Strupas, K. (2020). Results of the double-blind randomized controlled trial comparing laser hemorrhoidoplasty with sutured mucopexy and excisional hemorrhoidectomy. International Journal of Colorectal Disease, 35(3), 481-490.
Proßt, R. (2019). Short- and long-term results after laser haemorrhoidoplasty. coloproctology, 41(6), 446-447.
Salfi, R. (2009). A New Technique for Ambulatory Hemorrhoidal Treatment. coloproctology, 31(2), 99-103.
Valente, M. (2011). The Hemorrhoid Laser Procedure Technique vs Rubber Band Ligation: A Randomized Trial Comparing 2 Mini-invasive Treatments for Second- and Third-degree Hemorrhoids. Diseases of the Colon & Rectum, 54(6), 693-698.
Weyand G, Theis CS, Fofana AN, Rüdiger F, Gehrke T. Laser haemorrhoidoplasty with the 1470-nm diode laser in the treatment of second- to fourth-degree haemorrhoidal disease - a cohort study of 497 cases.
DR. BERNHARD HOFER, FLORIAN LIEBL & COLLEAGUES
Specialists in surgery, proctology
Brienner Str. 13, D-80333 Munich, Germany
- info@darmsprechstunde.de
- 0049-89-292679
- Monday - Thursday: 08.00 - 13.00 and 14.00 - 18.00
- Friday 08.00 - 13.00
- Saturday - Sunday : closed
To protect your personal data, the connection to Google Maps has been blocked.
Click on Load map to unblock Google Maps.
By loading the map, you accept the privacy policy of Google Maps.
You can find more information about the privacy policy of Google Maps here Google - Privacy Policy & Terms of Use.
© 2021 Proctology Clinic Munich
