Haemorrhoids treatment
Widespread disease hemorrhoids
Haemorrhoids: How to treat, when is surgery necessary?
The American Society of Colon and Rectal Surgeons (ASCRS) reports that more than two-thirds of the population experience hemorrhoid symptoms at some point. In Germany, it is estimated that 3.3 million cases are treated each year. The market for medical devices for hemorrhoid surgery is growing 5.6% annually in the U.S. to a projected $1.2 billion in 2031 (TMR Inc. 2022). Approximately 2 - 3% of patients who go to the doctor with symptoms undergo surgery.
Hemorrhoids can seriously affect concentration and confidence at work, limit exercise, and make you feel insecure about your body. The good news is that we can offer a wide range of effective therapies. We can help you make a good decision about whether or not surgery is appropriate and necessary. Any surgery wants to be well thought out, because we don't have a "spare part" for the bowel outlet.
The current expert guideline presents the common treatment methods in a way that is largely understandable to laypersons and evaluated on the basis of evidence; a comparative overview of the guidelines in Europe and the USA can be found here.

And what is the optimal treatment? In addition to the stage of hemorrhoids, the most important criteria are the leading symptom (bleeding, feeling of pressure, oozing) and the extent of subjective impairment. It is also important whether and how long conservative treatment measures have helped in the past and whether there is a suspicion of a malignant change in the skin or mucosa.
Treat hemorrhoids yourself
For prevention and in the early stages: 10 simple tips
Stool regulation: Psyllium husks, macrogol, lactulose
Improve stool texture (stool consistency): The goal is to have a formed stool that is not too hard. Especially in painful conditions, patients often try to keep stool quite soft. However, stool that is too soft has a longer contact time with the skin and penetrates every tiny wound or niche in the mucosa, leading to inflammation. Soft stool is harder to control (stool smearing) and exerts less stimulus to void (with the possible consequence of voiding dysfunction). Proven measures are
- Swelling and dietary fibers (psyllium husks, healing clay, absorbents)
- Osmotic stool regulants (macrogol, lactulose)
- Probiotics (bacterial cultures to stabilize the intestinal microbiome)
- a sufficient amount to drink
- the exclusion of food intolerances (lactose, fructose, gluten, histamine) by dietary diary and/or examination by a gastroenterologist


Stool habits: Psyllium husks, macrogol, lactulose
- Go to the toilet if you have to and not if you want to. Take your time, time pressure and stress to activate the sympathetic nervous system, which reduces intestinal activity.
- Avoid extreme pressure on the toilet, a slight activation of the abdominal press at the beginning is allowed.
- Use physiological reflexes such as the gastrocolic reflex. Simply put, a filling of the stomach leads to an emptying stimulus in the rectum. Drinking a large glass of liquid in the morning after getting up makes it easier to "do business" before rushing into rush-hour traffic.
- Compensate for the design of northern European toilets, which promote comfortable sitting but tend to make defecation more difficult due to an awkward anorectal angle. Since the bestseller "Bowels with Charm", we know that a stool under the feet supports the natural position.
- Read the newspaper at the breakfast table or on the underground, not in the quiet lavatory. Prolonged "toilet sessions" increase the pressure in the haemorrhoidal circulation and should therefore be avoided.
- Use moist cotton pads (available in drugstores) instead of moist toilet paper (can cause allergies), use natural care (marigold ointment, zinc ointment, baths with oak bark extract).
How the proctologist treats
Conservative treatment: Sclerotherapy and rubber band ligation
Sclerotherapy: Conventional sclerotherapy according to Blond or Blanchard
This most frequently performed treatment without surgery has the goal of tightening and stabilizing the connective tissue. In the so-called sclerotherapy (sclerotherapy), a drug is injected into the area of the vessels leading to the hemorrhoids (Blanchard's method) or, as is preferred in Europe, directly under the mucosa(Blond's method), which leads to scarring fixation and shrinkage of the hemorrhoidal nodes. This procedure can be performed painlessly on an outpatient basis and is therefore used very frequently. It usually has to be repeated several times at intervals of a few weeks. Several months may pass before the symptoms have completely disappeared.
Complications are extremely rare with the superficial injection technique of small volumes. Serious tissue damage had been reported with the phenol-oil mixtures used in the past; the sclerosing agent used today (polidocanol, ethoxysklerol®) is low-risk and usually very well tolerated. Nevertheless, sclerotherapy should be avoided in inflammatory bowel diseases and during pregnancy.
Ligation: Rubber band ligation, GBL, Barron ligation
With the rubber band ligature, excess mucous membrane is tied off with a rubber ring, the tissue repels itself after one to two weeks. This reduces the size of the haemorrhoids and fixes them in their natural position by scarring. This measure must also not cause any pain, otherwise a different method of treatment must be chosen.
Like sclerotherapy, GBL can be performed on an outpatient basis in a few minutes. Local anesthesia is possible, but usually not necessary. One to two rubber bands are placed per treatment. The treatment is basically repeatable until a satisfactory result is achieved. The guideline recommends rubber band ligation as the method of choice for hemorrhoids II°.
Bleeding or post-operative bleeding are risks, especially if you are taking blood-thinning medications. The tied tissue can be uncomfortable until it is rejected, so it is advisable not to put more than one or two bands in one treatment session.
Patients with chronic inflammatory bowel diseases (Crohn's disease, ulcerative colitis) as well as with a weakened immune system or with a latex allergy should not undergo ligation treatment.

Non-invasive sclerotherapy with LASER: HeLP - Hemorrhoid Laser Procedure
A new approach to hemorrhoid treatment is the use of medium energy laser energy, which strengthens the connective tissue and shrinks the hemorrhoids, but remains below the pain threshold. The practical implementation is comparable to sclerotherapy. We perform this treatment on an outpatient basis using a proctoscopy with a local anaesthetic gel, an anaesthetic is not required. Our experience with this technique is very good, especially persistent bleeding often responds well to this treatment.
In search of the best surgical technique
Haemorrhoid surgery: When to operate, how to operate?
Remove hemorrhoids: Hemorrhoidectomy

If conservative treatment of haemorrhoidal complaints does not bring sufficient therapeutic success, or if severe complaints exist from the outset, the best method for the individual case must be chosen from the available haemorrhoid surgery procedures.
The conventional methods for removing enlarged haemorrhoids, such as open haemorrhoidectomy using the Milligan-Morgan method, are tried and tested, but are associated with large wounds, thus lengthy follow-up treatment and not always optimal functional results. For stage four haemorrhoids, there is sometimes no other choice in rare cases.
By the third stage, a number of procedures have become established in which the enlarged vascular cushions are treated not by surgical ablation but by internal fixation and sclerotherapy of the haemorrhoids using laser or radiofrequency energy.
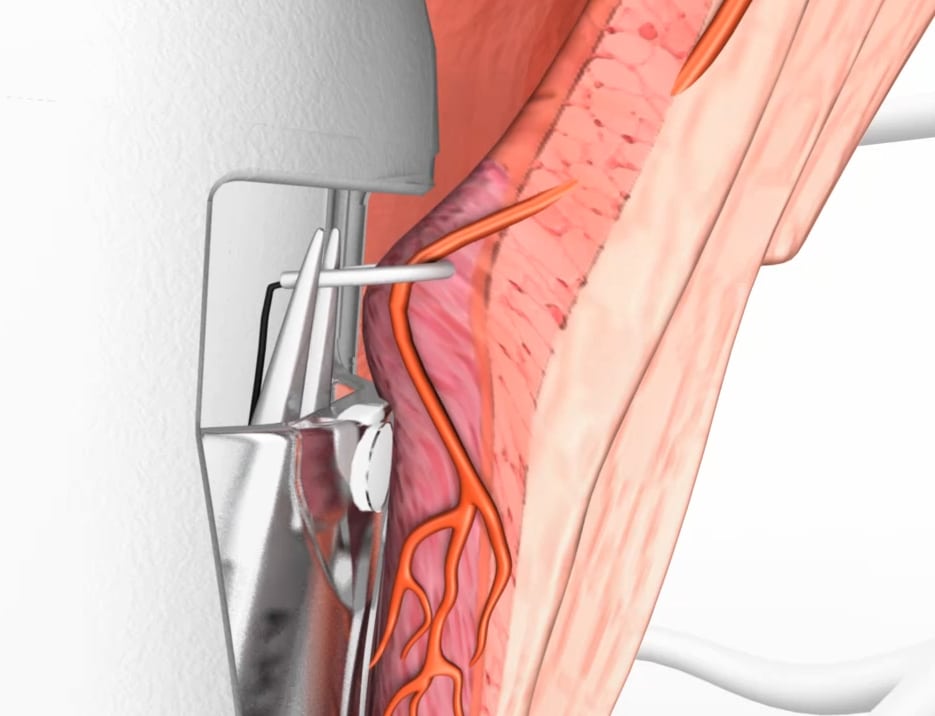
In the haemorrhoidal artery ligation according to Morinaga, the arteries supplying the haemorrhoids are cut off under ultrasound control. This suture can be continued as a spiral suture (recto-anal reconstruction), the combination of the two procedures is called HAL-RAR or Transanal Haemorrhoid Dearterialisation (THD).
Another elegant method of reducing third-degree haemorrhoids to normal size is sclerotherapy with laser (LASER haemorrhoidoplasty - LHP) or radiofrequency energy (RAFAELO method). In this procedure, the energy-applying probes are inserted into the centre of the haemorrhoid via access points of a few mm in size at the anal verge and the dilated vessels are shrunk by heat. In some centres, only local anaesthesia is even used for outpatient radiofrequency therapy.
Stabilize hemorrhoids: Stapling, suturing, laser
Stapler - hemorrhoidopexy (operation according to Longo)

In the Longo operation, a circular strip of mucosa is removed from the base of the haemorrhoidal ring, while at the same time connecting the edges of the cut with a ring-shaped staple suture. This both restricts the blood flow to the haemorrhoids and retracts the prolapse (hence the name stapler - haemorrhoidopexy, "fastening"). The staples heal into the scar or are gradually expelled. The procedure is widely used due to a short operation time as well as low-pain aftercare.
Hemorrhoid artery ligation (HAL, THD, Morinaga operation)
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Hemorhoids: Clinical classification
Individual therapy decision

"External hemorrhoid" - Mariske
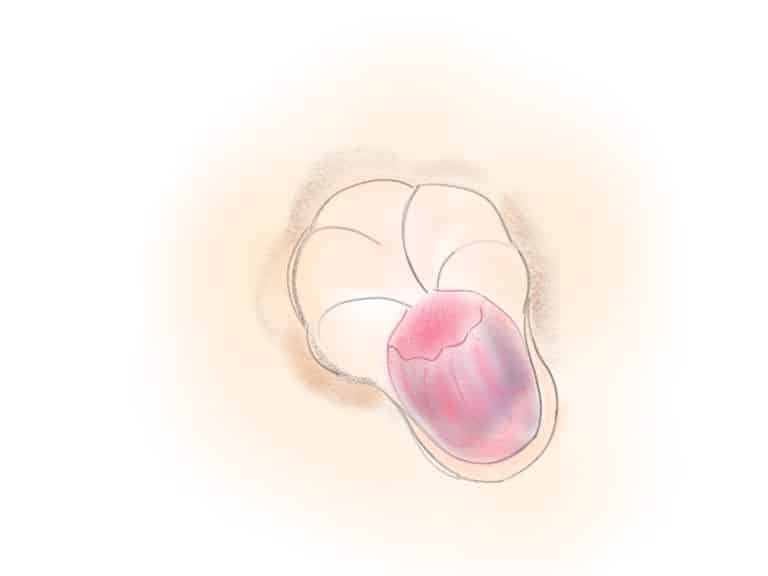
Single node (segmental prolapse)

Multiple nodes (circular prolapse)

Protrusion (eversion) of the anal canal
* Explanation to our short check
- Recommendation: Our subjective assessment of whether the procedure is generally recommendable
- Availability: the procedure is offered by at the proctologists of specialized centers
- I - IV°: Is the procedure suitable for the respective stages of the hemorrhoidal condition?
- Cash: Cost coverage by statutory health insurance
- Private: Cost coverage by private health insurance
- Self: Is the procedure offered to self-pay patients?
- IGV: Are there special contracts with statutory health insurers for the assumption of costs?
- Outpatient/Stat: Can the procedure be performed on an outpatient basis or does it require hospitalization?
- Anesthesia: do you need anesthesia for the treatment?
- Time: Treatment duration
- and lastly: Is the treatment repeatable if necessary?
And finally, the evidence to read again
Bibliography: Haemorrhoids treatment and surgery
- Davis, B. R., Lee-Kong, S. A., Migaly, J., Feingold, D. L., & Steele, S. R.. (2018). The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Diseases of the colon and rectum, 61(3), 284-292.
- Furtwängler, A. (2020). Sclerotherapy. coloproctology, 42(1), 14-17.
- Muldoon R. (2020). Review of American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. JAMA surgery, 155(8), 773-774.
- Petersen, S., Holch, P., & Jongen, J. (2020). Guidelines for the treatment of haemorrhoidal disease. coloproctology, 42(1), 6-13.
- Trompetto, M., Clerico, G., Cocorullo, G. F., Giordano, P., Marino, F., Martellucci, J., Milito, G., Mistrangelo, M., & Ratto, C. (2015). Evaluation and management of hemorrhoids: Italian society of colorectal surgery (SICCR) consensus statement. Techniques in coloproctology, 19(10), 567-575.
