How to tell if you have haemorrhoids
The 5 most common symptoms
Itching
Why does itching occur? Haemorrhoids are located in the transition zone from the mucous membrane of the rectum to the normally dry, outer skin. As the name suggests - mucous membrane produces mucus. Enlarged haemorrhoids can block the sphincter muscle like "the foot in the door", allowing the passage of mucus and moisture onto the skin. The result is skin irritation (irritant anal eczema). When the slightly damaged skin loses its barrier function, it becomes more susceptible to intestinal bacteria and digestive enzymes in the stool. The process takes on a life of its own.
In some skin diseases (psoriasis, neurodermatitis), isolated infestation of the pre-damaged skin in the area of the anus is also found for this reason.
Bleeding
Blood in the stool is considered an alarm symptom for bowel cancer and therefore often leads to uncertainty. However, the vast majority of all bleedings have benign causes. The type of bleeding gives clues about the probable cause: slight traces of bright red blood on the toilet paper are often signs of eczema or enlarged haemorrhoids. An anal fistula or coccygeal fistula can also cause such traces of blood. Dripping bleeding is typical of anal fissure. Blood admixtures to the stool or clotted blood is suspicious of a source of bleeding in the colon. The proctologist will therefore first perform an endoscopy of the rectum and treat any visible source of bleeding. To be on the safe side, he will usually arrange for a colonoscopy to remove any doubts about the cause of the bleeding.
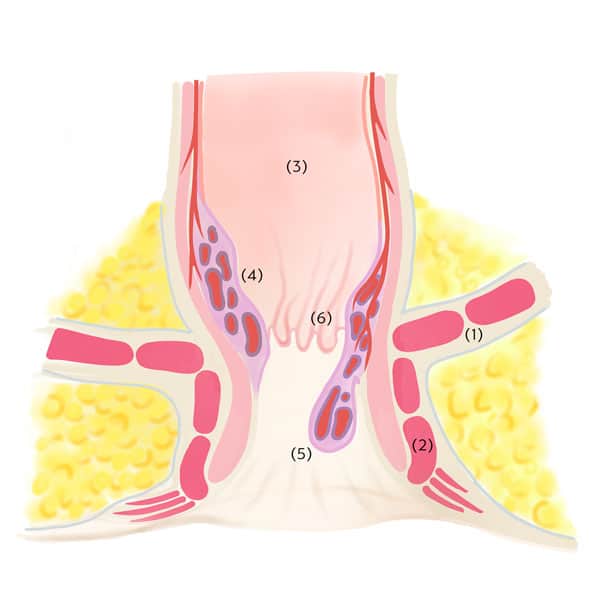
Protrusions
The reduction or loss of stability of the connective tissue can cause a haemorrhoidal knot to become mobile in relation to the sphincter and the muscles of the bowel wall. The knot can then protrude from the rectum when going to the toilet or spontaneously. If such a prolapse recedes on its own, it is called stage II; if it has to be pushed back, it is called stage III of haemorrhoidal disease. The protrusion of the haemorrhoid leads to disruption of the fine seal (regreasing, laundry soiling) and dampness around the anus. This in turn can cause skin irritation (irritant anal eczema) with itching and soreness.
Stool smearing, moisture
The haemorrhoids are actually a useful part of the so-called continence organ and, in interaction with the sphincter muscle, provide the fine seal. If the haemorrhoids become enlarged or displaced, this fine continence can suffer. Patients then complain of secretion of moisture or stool smearing. This symptom usually has nothing to do with a real weakness of the sphincter muscles. Often, optimising the composition of the stool (building up the intestinal flora, plant-based bulking agents) is enough to restore normal function. Treatment can then be limited to stabilising the connective tissue by sclerotherapy.
Feeling of pressure
The sensitive receptors of the rectum cannot always distinguish whether the bowel is full or whether it is just enlarged haemorrhoids causing a feeling of pressure or foreign bodies in the anal area. Patients then often repeatedly go to the toilet and try to empty themselves by pressing harder. Understandably, this is counterproductive in this situation, as the increase in pressure causes the haemorrhoids to swell further and be pushed downwards, so that the discomfort even increases. This symptom can often be treated very effectively with simple remedies.